Mental health is your mental/emotional state that helps you cope with the ups and downs of life every day. Your mental health can be affected by several things, including brain injury.
You might be struggling with your mental health because:
- Your brain injury has changed your life
- There’s damage to the parts of the brain that control your mental health and emotions
- You’ve experienced trauma
- You have been diagnosed with a disorder connected to anxiety, depression or even post-traumatic stress
These are just a few examples. Pretty much everyone struggles with their mental health at some point. When that happens, it’s important to rely on your support system. This could be your parent(s), teachers, doctors, or therapists.
Your mental health is an important part of your well-being because it directly impacts how you feel and your capacity for relationships, activities, and more. Taking care of your mental health is an ongoing process, and it’s something you may need help with for the rest of your life (even if most of the time you have positive mental health).
Let’s talk about:
Preventative mental health
Have you ever heard the proverb “an ounce of prevention is worth a pound of cure?” It means that (in most cases) it’s easier to keep something from happening than it is to stop it after it’s started [1]. This is true for a lot of things, and that can include your mental health.
Remember: Mental health is an important part of your life and can be complicated. While prevention of mental health problems is helpful, it’s also okay if some things can’t be prevented. Wherever you are with your mental health, there are resources and people that can help.
The way brain injury can impact your mental health is something we talk about a lot, because it impacts how you think and feel about yourself, your family, your life and the world around you. It’s also really important for people your age to be talking about mental health because research shows that over 70% of people who have a mental illness have symptoms before the age of 18 [2].
You aren’t going to feel happy and positive all the time (that’s not realistic). But the goal with preventative mental health practices is to help you have a positive sense of mental health and give you the tools/resources to cope when you aren’t feeling positive.
In 2015, the Youth Council at the Mental Health Commission of Canada created a youth perspective on the Mental Health Strategy that was released in 2013. This includes six strategic directives, one of which is “Encourage lifelong mental health in all social environments where people live or spend time and prevent mental health issues and suicide wherever possible” [3]. The priorities for this directive include:
- Reducing stigma about mental health (so people understand it more and feel more comfortable asking for help).
- Making sure the adults in a youth’s life have the necessary information and tools about mental health and how to read early signs of mental health issues.
They also discuss the importance of being able to access supports and remove barriers (like the cost of supports) so that everyone who needs help can get it.
There are a lot of different ways you can support your mental health both through mindful mental-based activities and through taking care of your physical health. You can find out more information on the following pages:
Remember: everyone’s mental health is different. Some more specific, day-to-day tools/supports may work for you but not for someone else (or the other way around). It’s best to ask your parent/guardian and health care team for more information.
How do I know if I’m struggling with my mental health?
Signs of potential mental health issues can include [4]:
- Changes in sleeping/eating patterns
- Changes in your mood
- Getting angry or upset more quickly
- Difficulty coping with stress
- Difficulty concentrating on things like school
- Changes in how you see yourself/your physical appearance
- No longer wanting to be around friends or other people
- Fatigue
- Changes in weight
- Hearing or seeing things that aren’t there
- No longer doing things you used to really like
Everyone has mental health issues from time to time, but it becomes a problem when these kinds of symptoms don’t stop and prevent you from living your life. Your health care and support team can help you determine what’s prompting your feelings and how to manage them moving forward.
What’s the difference between mental health and mental illness?
As we’ve talked about, mental health is the state of being where you can process emotions, thoughts, and feelings. Depending on what’s going on in your life, you can have good mental health or bad mental health. Just like with most things, there’s ups and downs. Many Canadians will have periods of time where they struggle with their mental health.
Your mental health can be influenced by several factors including:
- Significant life changes
- Relationships
- Isolation
- Physical health
- Age
- Gender
- Stress
- Trauma
- Employment
Mental health is different from a mental illness. You might have heard these terms used and thought they were basically the same. But a mental illness is a diagnosed disorder that impairs how you think, feel, behave, or interact with others. Examples of mental illnesses include:
- Addiction (problematic use) disorders
- Anxiety disorders
- Eating disorders
- Mood disorders like depression or bipolar
- Personality disorders
- Post-traumatic stress disorder
- Psychosis disorders like schizophrenia
Studies have shown that individuals with a brain injury have a higher chance of developing a mental illness. A mental illness can only be diagnosed by professionals such as psychologists, psychiatrists and family doctors [5].
While you may have symptoms of some of these disorders, that doesn’t mean you have a mental illness. And if you do have a mental illness, that doesn’t mean you can’t have good mental health. Any questions about this should be shared with your doctor [6].
Common mental health challenges
Many people will experience mental health challenges, as as we’ve talked about, your brain injury and mental health may be tied together in some cases. Here are some of the mental health challenges you may have.
Remember
Mental health is different for everyone, and just because these are common challenges doesn’t mean you will experience them (or that you won’t experience other challenges with mental health). It’s always best to talk to your doctor about your mental health questions.
Anxiety
Anxiety is feelings of worry and fear, most often about the unknown. It’s normal to experience some anxiety, especially as you recover from a brain injury and have new experiences—but it becomes problematic when:
- You’re unable to calm your anxiety
- You get anxious when there’s nothing that should be causing you anxiety
- You get anxious really quickly and out of nowhere
- You get overwhelmingly anxious in response to something small
There are a few different types of anxiety you can experience including general anxiety and social anxiety. General anxiety means you experience regular anxiety (often way more than the situation needs) throughout your day/the different parts of your life. You may find your anxiety difficult to cope with. Social anxiety often means you feel fearful and stressed about social interactions with family and friends or strangers. You may even avoid situations where you have to talk to others or if you feel like people are watching you. There’s a lot of worries about being embarrassed or rejected. These worries can cause someone to become socially isolated [7].
Coping with anxiety
Anxiety is a normal bodily response, so you’re never going to eliminate it—and you shouldn’t try to! Like we mentioned earlier, a little anxiety can be good because it’s alerting us to danger. But you still need to know how to manage your anxiety, especially if you’re feeling it when there isn’t any danger.
First: what’s causing your anxiety? If you spend a lot of your time feeling worried and anxious, it may be helpful to keep a daily journal to document when you start feeling anxious and what triggers it. You can do this on your smartphone, a computer or in a notebook you carry with you.
When you do start to feeling yourself getting worried, you can try a few different techniques to start calming down.
- Ask for help from people you know and trust. You don’t have to try to figure this out on your own.
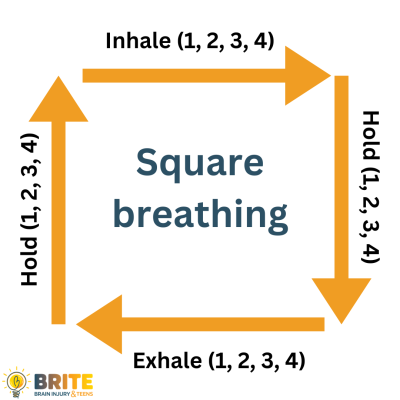
- Deep, conscious breathing. We spend most of our time breathing without thinking about it. But taking deep breaths with intention can help you get in touch with how you’re feeling and how you want to feel. We’ve got a couple breathing resources at the end of this list.
- Pay attention to the different parts of your body and make them as relaxed as you can. You may find you’ve been clenching your jaw or hunching your shoulders because you’re anxious.
- Set goals for yourself (broken up into small steps) to help you address what makes you anxious. For example, does taking the bus make you anxious?
- Break down the different steps of that process, and practice them one by one.
- Use checklists to help you understand what may happen, and remember important things (that can be a big source of anxiety for a lot of people).
Resources
Try our square breathing exercise.
- Breathing exercise video
- Self-help strategies for anxiety—Anxiety Canada (remember, only a doctor can diagnose disorders)
- Anxiety Canada resources
- Here to Help BC – Youth Mental Health resources
Depression
Depression is an emotional/mental state where you feel sad, uninterested in activities or parts of your life you normally enjoy, and/or stop engaging with the people in your life [8]. It can be an intense mental health challenge.
Important
A lot of people say “I’m depressed” to describe the state of their mental health. However, it’s important to know that there’s a difference between feeling depressed (which is something that many people experience) and having major depressive disorder. Only a medical professional can provide a diagnosis of depression. But that doesn’t mean people who don’t have a diagnosis don’t feel the symptoms and effects of depression. It’s always best to talk to a professional about depression.
Depression can be caused by your emotional state/what you’re going through in life. This most often connects to grief and ambiguous loss. It can also be caused by physical changes in/to your brain [9]. Symptoms of depression can include:
- Changes in eating patterns
- Changes in sleep
- Changes in weightFeelings of sadness
- Focus on the emotions of loss and grief
- Helplessness, worthlessness, and guilt
- Irritability
- Less interest or pleasure in the hobbies you previously enjoyed
- Physical aches and pains
- Poor concentration
- Tiredness or loss of energy
- Thoughts of death and suicide
- Removing yourself from friends and family
Keep in mind
You may have some of these symptoms and not have depression. Talk to your health care team about any emotional or physical symptoms you may be experiencing. If you experience symptoms for a long period of time or suspect that your depression isn’t related to grief/ambiguous loss, you should see a medical professional who can diagnose depression.
Extended periods of depression can have an impact on your recovery. You may be more fatigued, have trouble engaging with people, or find participating in rehabilitation harder. You may also have trouble recognizing when you’re depressed and not have the skills to cope with it in a constructive way.
If you are diagnosed with depression, you may be prescribed medication and/or various therapies (this will be talked about with your doctor). Some things you can do at home to cope with depression and support your mental health include [9]:
- Following a balanced diet
- Engaging in physical activity
- Finding enjoyable hobbies like crafting, painting, video games, or reading
- Getting an appropriate amount of rest
- Meditation
- Talking to friends and family
Again, there are lots of supports and tips out there. Make sure to ask parents and your health care team for advice and help figuring out what supports feel good for you.
Post-traumatic stress disorder (PTSD)
Post-traumatic stress disorder (PTSD) is a mental health disorder that can occur in people who have suffered or seen a traumatic event. This event could be anything traumatic, like an accident or an assault.
Symptoms of PTSD can include:
- Anxiety
- Increase in negative thoughts, feelings, and beliefs stemming from the trauma
- Disassociation – losing touch with the present and feeling like you are experiencing the trauma again
- Hallucination flashbacks to the event
- Nightmares
- Avoidance of certain situations that may recall the trauma
- Feeling on guard all the time
- Not remembering parts of the trauma
- Sleep problems
Not every person who suffers a traumatic brain injury will have PTSD and not everyone with PTSD will have a brain injury. It depends on the person, their injuries, and how the trauma was processed. Only a licensed professional like a psychologist or psychiatrist can diagnose PTSD [10].
Panic attacks
Sometimes people with anxiety or PTSD can have panic attacks. These are sudden surges of intense discomfort that reach a high within minutes. Signs of a possible panic attack can include:
- Feelings of choking, chest pain, nausea, dizziness
- Feelings of detachment or unreality
- Heart palpitations
- Hot or cold flashes
- Numbness or tingling
- Shakiness or trembling
- Shortness of breath
- Sweating
A panic attack can be brought on by different things, but they often happen when you’re feeling trapped or overly anxious about something. You may spend a lot of time scared you’ll have another one, so you isolate yourself or stick to ‘safe’ environments, which can impact how you live your life.
Ways to cope with panic attacks include:
- Calm breathing
- Body relaxation, where you tense up a muscle and release it
- Identifying your triggers
- Imagining a person, place, or thing that is powerful enough to calm your mind
- Using cards that remind you of coping strategies
- Talking to a therapist
- Slowly building up your tolerance to the triggers that start your panic attacks
Resources
- More information on post-traumatic stress disorder from Anxiety Canada
- Anxiety Canada has a helpful guide on coping with panic disorders (which can include panic attacks).
- MindKit is a resource created for young family members of Canadian Veterans to cope with and learn about post-traumatic stress injury (PTSI)
Before you keep reading
This next section talks about suicide and suicidal thoughts. This is something that’s important to talk about, but you may not be in a place where you can read about it. If you are looking for helplines or crisis supports, this link will take you down to the bottom of the page past the information section. We have also linked more information from Kids Help Phone and other organizations committed to helping youth.
Suicidal thoughts
After a brain injury, you may experience lasting changes to your personality, abilities, relationships, and how you process information (including impulse control). These changes can be hard, and lead to feelings of loneliness, hopelessness and anger. This (along with other factors) may lead to a higher risk of suicidal thoughts. Signs of suicidal thoughts include:
- Statements about dying or wishing to have died
- Isolation or withdrawal from others
- Intense feelings of hopelessness and helplessness
If you are experiencing suicidal thoughts, talk to your doctor, therapist, parent, or call a helpline immediately.
- Kids Help Phone
- Call 9-8-8: Suicide prevention helpline
Reaching out for help will improve your mental health. No matter how unbearable it feels right now it won’t last forever. With time and support you’ll feel better, which is why it’s important you confide in your family, health care team, and anyone else you trust. You’re never alone, the people around you want to help.
It’s important to remember that these thoughts and feelings can happen even a long time after your brain injury. It’s important to regularly check in with yourself and your family/friends about your mental health and how you’re feeling.
Disclaimer: There is no shortage of web-based online medical diagnostic tools, self-help or support groups, or sites that make unsubstantiated claims around diagnosis, treatment and recovery. Please note these sources may not be evidence-based, regulated or moderated properly and it is encouraged individuals seek advice and recommendations regarding diagnosis, treatment and symptom management from a regulated healthcare professional such as a physician or nurse practitioner. Individuals should be cautioned about sites that make any of the following statements or claims that:
- The product or service promises a quick fix
- Sound too good to be true
- Are dramatic or sweeping and are not supported by reputable medical and scientific organizations.
- Use of terminology such as “research is currently underway” or “preliminary research results” which indicate there is no current research.
- The results or recommendations of product or treatment are based on a single or small number of case studies and has not been peer-reviewed by external experts
- Use of testimonials from celebrities or previous clients/patients that are anecdotal and not evidence-based
Always proceed with caution and with the advice of your medical team.
Information for this section provided in part by the Acquired Brain Injury Partnership Project.
[1] Merriam-Webster
[2] Children and Youth—Mental Health Commission of Canada
[3] The Mental Health Strategy for Canada: A Youth Perspective—Mental Health Commission of Canada
[4] Children and youth mental health: signs and symptoms—Government of Ontario
[5] Looking for Mental Health Services—Centre for Addiction and Mental Health
[6] Here to Help BC
[7] Anxiety Canada
[8] Depression–MyHealthAlberta
[9] Model Systems Knowledge Translation Centre, Depression After Traumatic Brain Injury
[10] Post Traumatic Stress Disorder—Anxiety Canada